What is breast cancer?
Breast cancer is a complex and varied disease, and what it feels like can vary greatly depending on the individual and the stage of the cancer. It’s important to note that not all breast cancer cases present with noticeable symptoms, and some are only detected through routine screening like mammograms. However, here are some common signs and sensations associated with breast cancer:
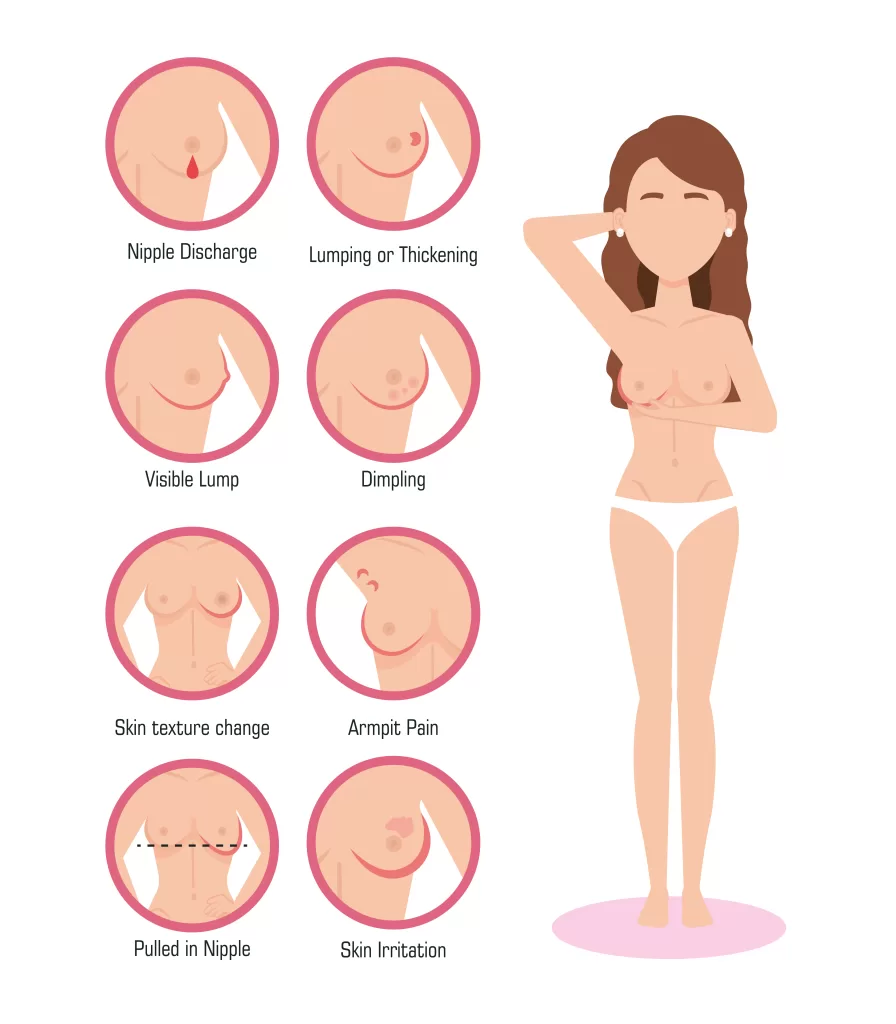
- Lump or Thickening: One of the most common early signs of breast cancer is the presence of a lump or thickening in the breast tissue. This lump is often painless but can be tender or painful in some cases. It’s important to remember that not all breast lumps are cancerous, but any new lump should be evaluated by a healthcare professional.
- Breast Pain: It can sometimes cause breast pain or discomfort, but this is not always present. Pain is more commonly associated with benign breast conditions, but it’s essential not to dismiss it without evaluation.
- Changes in Breast Size or Shape: Breast cancer can lead to changes in the size or shape of the breast. This may be noticeable when comparing one breast to the other or over time as the cancer progresses.
- Skin Changes: Changes in the skin of the breast can be a sign of breast cancer. This may include redness, dimpling, puckering, or the appearance of an orange peel texture.
- Nipple Changes: Changes in the nipple, such as inversion (pulling inward), discharge (other than breast milk in breastfeeding women), or a change in appearance, can be a sign of breast cancer.
- Swelling or Thickening in the Underarm: Breast cancer can affect the lymph nodes in the underarm area (axilla), leading to swelling or thickening.
It’s essential to understand that many of these symptoms can also be caused by benign breast conditions, so experiencing one or more of these symptoms does not necessarily mean you have the condition.
Will it show up in blood work?
It is typically not diagnosed through routine blood work alone. While blood tests can provide some information about a person’s health, they are not the primary method for diagnosing breast cancer. The diagnosis typically involves a combination of various methods, including:
- Mammography: A mammogram is an X-ray of the breast tissue and is commonly used for breast cancer screening. It can detect suspicious abnormalities or masses in the breast.
- Clinical Breast Examination (CBE): A healthcare provider performs a physical examination of the breasts to check for lumps, changes in texture, or other abnormalities.
- Breast Ultrasound: Ultrasound imaging is often used to further evaluate breast lumps or abnormalities detected during mammography or CBE.
- Biopsy: If an abnormality is found, a biopsy is performed to collect a sample of tissue from the suspicious area for laboratory analysis. This is the definitive method to confirm whether cancer is present and what type it is.
- Blood tests may be used in the management of thet cancer, but they are not used for primary diagnosis. They can provide information about a person’s overall health, check for markers associated with it, and monitor the effects of treatment, but they do not directly detect cancer cells
Some blood tests, such as those that measure tumor markers like CA 15-3 and CA 27.29, may be used to monitor the progress of the cancer treatment or to detect recurrences in some cases. However, these markers are not specific to breast cancer and can also be elevated in other conditions.
Are breast cancer lumps painful?
Breast cancer lumps can vary in terms of pain or discomfort. Some lumps are not painful at all, while others can be tender or cause discomfort. The presence of pain or discomfort in the breast does not necessarily indicate breast cancer, as many benign (non-cancerous) conditions can also cause breast pain.
It’s essential to understand that it can present in different ways, and not all cases involve a noticeable lump. Other signs and symptoms of breast cancer can include changes in breast size or shape, nipple discharge (other than breast milk), skin changes on the breast, or persistent pain in the breast or nipple
Can you have breast cancer without a lump?
Breast cancer can manifest in various ways, and not all cases present with a noticeable lump. While breast lumps are a common symptom of breast cancer, there are other signs and symptoms to be aware of. It’s important to remember that many of these symptoms can also be caused by non-cancerous conditions, so having any of these symptoms doesn’t necessarily mean you have it. However, if you notice any changes in your breast health, it’s essential to consult a healthcare professional for a proper evaluation. Some signs and symptoms of breast cancer without lumps include:
- Changes in Breast Skin: Redness or rash on the breast or nipple. Dimpling or puckering of the breast skin, resembling orange peel. Swelling or thickening of the breast skin.
- Nipple Changes: Inversion or retraction of the nipple or discharge from the nipple, which may be bloody.
- Breast Pain: Unexplained pain in the breast or nipple that doesn’t go away.
- Changes in Breast Size or Shape: Noticeable changes in the size, shape, or contour of the breast.
- Swelling or Enlargement: Swelling or enlargement of one breast compared to the other.
- Skin Texture Changes: Changes in the texture of the breast skin, such as it becoming scaly.
How can I lower my chances of getting breast cancer?
Lowering your risk of cancer involves adopting a combination of lifestyle changes and healthcare strategies. While it’s not always possible to prevent it entirely, these steps can significantly reduce your risk:
- Maintain a Healthy Weight
- Eat a Healthy Diet
- Be Physically Active
- Breastfeeding
- Hormone Replacement Therapy (HRT)
- Know Your Family History
- Regular Screening
- Self-Exams
- Avoid Environmental Toxins
- Stay Informed
Breast cancer for men?
Breast cancer can affect both men and women, although it is much more common in women. Breast cancer in men is relatively rare, accounting for less than 1% of all cases. Because of its rarity in men, it is often not top of mind when discussing cancer risks for males, but it is essential to be aware of the possibility and understand the basics.
Here are some key points about breast cancer in men:
- Risk Factors: Some risk factors for male breast cancer include:
- Age: The risk of cancer increases with age.
- Family History: A family history of breast cancer, especially in first-degree relatives (such as a mother, sister, or daughter), can increase the risk.
- Inherited Gene Mutations: Mutations in the BRCA1 or BRCA2 genes, which are associated with breast and ovarian cancer, can also increase the risk in men.
- Hormone Imbalance: Conditions that lead to an imbalance of hormones, such as Klinefelter syndrome or cirrhosis, can be associated with male breast cancer.
- Radiation Exposure: Prior exposure to chest radiation, such as for the treatment of another cancer, can increase the risk.
- Signs and Symptoms: The most common symptom of male breast cancer is a painless lump or swelling in the breast tissue. Other symptoms may include nipple discharge (often bloody), changes in the size or shape of the breast, or changes in the skin over the breast.
In conclusion, breast cancer remains a significant health concern, but strides in research, early detection, and treatment options have provided hope for countless individuals and their families. While the journey through the issue can be challenging, the power of awareness, regular screenings, and ongoing support cannot be underestimated. By continuing to raise awareness, invest in research, and prioritize preventive measures, we can aspire to a future where breast cancer is not only treatable but ultimately preventable. Together, we can work towards a world where the fear of breast cancer is replaced with confidence in our ability to detect and combat this disease effectively, offering brighter prospects for those affected and their loved ones.
Come on down to MedConsult Clinic to have an extensive breast cancer checkup! If you would like to read our other articles click here! You can message us thrugh out Whatsapp, 064-350-4438, or you can contact us through our LINE, @medconsultclinic!

